As states institute opioid policies to address the opioid epidemic, a new study has found considerable decreases in the prevalence of longer-term dispensing of opioids to injured workers in a number of states studied.
The study, Longer-Term Dispensing of Opioids, 4th Edition, by the Workers Compensation Research Institute (WCRI), examined trends of longer-term dispensing of opioids in 26 state workers’ compensation systems. It also documents how often the services such as drug testing, psychological evaluation and treatment recommended by treatment guidelines were used for managing chronic opioid therapy.
WCRI released this sample of the study’s findings:
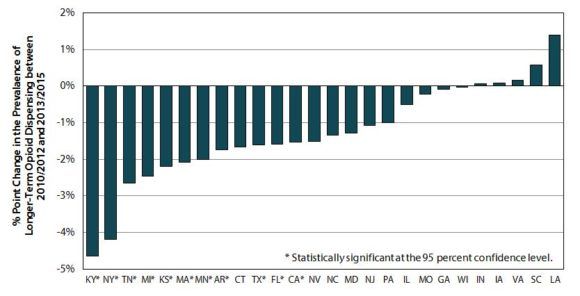
- The frequency of claims that received opioids on a longer-term basis decreased more than four percentage points in Kentucky and New York. The same measure decreased two to three percentage points in several other states (Kansas, Massachusetts, Michigan, Minnesota and Tennessee). Noticeable decreases in the longer-term dispensing of opioids were also seen in several other states, including California, Florida and Texas, with reductions of one to two percentage points.
- Among claims with injuries in 2013 that were observed over a two-year time period ending March 2015, longer-term dispensing of opioids was most prevalent in Louisiana—1 in 6 injured workers with opioid prescriptions were identified as receiving longer-term opioids. Compared with most study states, the number was also higher in California, Georgia, North Carolina, Pennsylvania, South Carolina and Texas. By contrast, about 1 in 25 injured workers with opioid prescriptions received them on a longer-term basis in Indiana, Kansas, Missouri, Nevada, New Jersey, and Wisconsin.
- The study continued to find that fewer than expected injured workers who received opioids on a longer-term basis had certain services (i.e., drug testing, psychological evaluation and treatment, etc.) recommended by treatment guidelines for chronic opioid management. For example, in 19 out of 26 states, less than 10 percent of injured workers with longer-term opioids received psychological evaluations.
“Research finds that high doses and prolonged use of opioids may lead to addiction, increased disability or work loss, and even death,” said Ramona Tanabe, WCRI’s executive vice president and counsel. “The information in this report can help policymakers and other stakeholders compare the trend of longer-term dispensing of opioids in their state to other states, and learn what policy tools are available to reduce unnecessary opioid use.”
This study used data comprising more than 400,000 nonsurgical workers’ compensation claims with more than seven days of lost time; more than two million prescriptions are associated with these claims from 26 states. These claims had injuries in 2010 and 2013 and received on average up to 24 months of medical treatment. The sample of claims in the study represents 36–69 percent of workers’ compensation claims in each state.
The 26 states in the study are Arkansas, California, Connecticut, Florida, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Nevada, New Jersey, New York, North Carolina, Pennsylvania, South Carolina, Tennessee, Texas, Virginia and Wisconsin.
The Workers Compensation Research Institute (WCRI) is an independent, not-for-profit research organization based in Cambridge, Mass. Its members include employers, insurers, governmental entities, managed care companies, health care providers, insurance regulators, state labor organizations and state administrative agencies in the U.S., Canada, Australia and New Zealand.
Topics California Texas Claims Workers' Compensation Talent Kansas
Was this article valuable?
Here are more articles you may enjoy.


 Marsh McLennan Agency to Buy Fisher Brown Bottrell for About $316M
Marsh McLennan Agency to Buy Fisher Brown Bottrell for About $316M  AIG General Insurance Chairman McElroy to Retire May 1
AIG General Insurance Chairman McElroy to Retire May 1  Why New York’s Attorney General Objects to Trump’s Bond Insurer
Why New York’s Attorney General Objects to Trump’s Bond Insurer  Survey Shows Majority of Florida, California Homeowners Seeing Higher Insurance Costs
Survey Shows Majority of Florida, California Homeowners Seeing Higher Insurance Costs 

