

Texas workers’ compensation claims handled through health care networks have lower medical costs than those managed outside networks, a state report finds.
The Texas Department of Insurance has published its 2020 Workers’ Compensation Network Report Card Results showing networks outperform non-networks on various measures including medical costs per claim for injured workers.
“Overall, the 2020 network report card continues to show that networks tend to be more cost-efficient than non-network claims, and these cost differences appear to be partially driven by lower hospital utilization and lower prices per service. Despite lower costs, network claims generally have better return-to-work and functional outcomes, compared with non-network claims,” the report concludes.
Network claims also tend to receive initial non-emergency medical care sooner than non-network claims, which may help in controlling medical costs and reducing unnecessary disability among injured employees.
The results in the annual report card show a comparison of 11 groups, 10 of which are networks, with a total of 110,515 new injured employees with injuries occurring between June 1, 2018, and May 31, 2019.
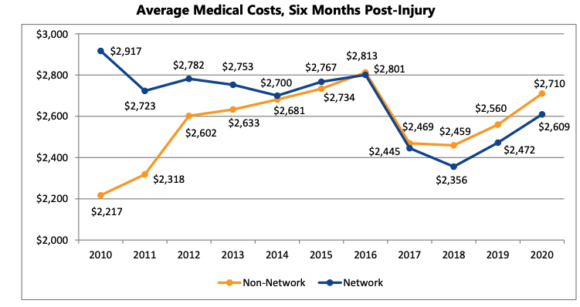
According to the report, the medical costs picture has changed. From 2010 to 2016, networks had higher average medical costs per claim for initial care, compared to non-network claims. However, since 2017, non-network average medical costs per claim at six months post-injury have been approximately 4 percent higher on average than network claims.
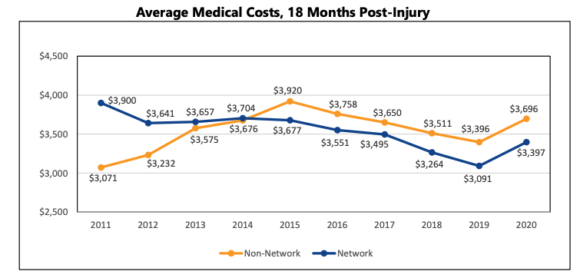
The report shows the medical cost gap widening between network and non-network claims at 18 months post-injury. Network medical costs were about 9 percent lower per claim at 18 months post-injury compared with non-network claims.
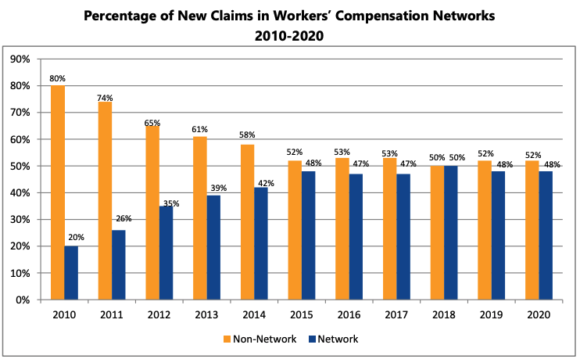
Networks’ participation in treating workers’ compensation claimants appears to have stabilized. Almost half of all new claims are treated in networks, and the percentage of new claims treated in networks has not changed significantly since 2015.
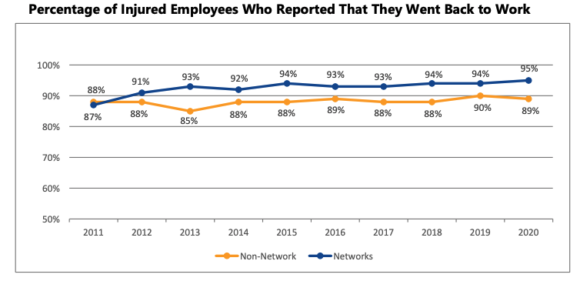
A higher percentage of network claims report returning to work after their injuries: Since 2012, network claims consistently report higher return-to-work rates than non-network claims.
Other findings include:
The report looks at results from 11 groups: WorkWell (37,991), 504-Alliance (20,981), Coventry (11,755), Sedgwick (5,727), Travelers (5,654), IMO (4,430), Liberty (3,412), First Health (3,116), Corvel (2,557), and all other networks (14,892) relative to the non-network injured employees (120,337).
There are 30 networks covering 254 Texas counties that are certified to provide workers’ compensation health care services to insurance carriers as of June 1, 2020. Twenty-one certified networks actively treated injured employees as of May 31, 2019. Since 2006, about 1.1 million injured employees have been treated in workers’ compensation networks.
The report advises that not all networks are the same. The report card shows differences by individual networks’ performance in injured employees’ perceptions about their access to care, satisfaction with care and other measures.
Source: The 2020 Workers’ Compensation Network Report Card Results.