There is new evidence that ambulatory surgery centers are less expensive for certain surgeries than hospitals.
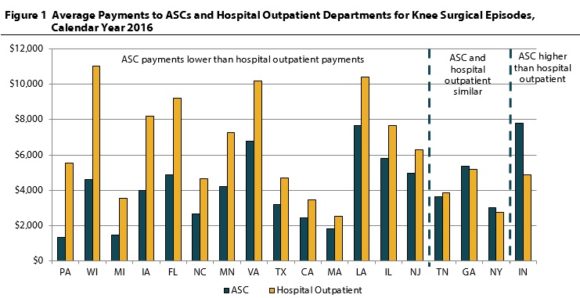
Payments for similar knee and shoulder surgeries performed in ambulatory surgery centers (ASCs) were lower compared with hospital outpatient departments in 14 of 18 states studied, according to a new report from the Workers Compensation Research Institute (WCRI).
“Some studies indicate that ASCs provide care that is less expensive than services provided in hospitals,” said Ramona Tanabe, WCRI’s executive vice president and counsel. “This analysis is important since evidence about ASC surgeries from other payors (Medicare or group health insurance) may not apply in workers’ compensation settings.”
According to the report, in 14 states, payments for knee surgeries done at ASCs were at least 21 percent lower than payments for hospital outpatient surgeries in 2016. In three states, the payments were similar, and in Indiana, payments for ASC surgeries were 59 percent higher than payments for hospital outpatient surgeries. Similar results were found for shoulder surgeries.
The authors – Dr. Bogdan Savych and Dr. Rebecca Yang – examined payments to ASC and hospital outpatient departments by looking at the most common groups of surgeries conducted in outpatient settings—knee and shoulder arthroscopies.
The study shows information on all payments to these two types of facilities – ASCs and hospital outpatient departments– within a surgical episode, but excludes payments to surgeons or other medical professionals.
The authors note that the differences in payments for ASC and hospital outpatient surgeries may be attributed to multiple factors, such as a state’s fee schedule regulations, network participation rates, or negotiated prices. For example, in Indiana, payments for hospital outpatient surgeries are reimbursed at 200 percent of Medicare after the adoption of a hospital fee schedule in 2014, while payments to ASCs remain unregulated.
Changes in states’ fee schedules affected the trends in ASC payments for surgeries in a number of states. For example, in North Carolina, average payments for knee surgeries decreased 55 percent between 2012 and 2016. In New York, average payments for knee surgeries increased 50 percent between 2015 and 2016.
The 18 states included in this study, WCRI FlashReport: Comparing Payments to Ambulatory Surgery Centers and Hospital Outpatient Departments, are California, Florida, Georgia, Illinois, Indiana, Iowa, Louisiana, Massachusetts, Michigan, Minnesota, New Jersey, New York, North Carolina, Pennsylvania, Tennessee, Texas, Virginia, and Wisconsin. They were selected because they are geographically diverse; represent a range of system features; and represent the range of states that are higher, near the middle, and lower on costs per claim.
Topics Workers' Compensation
Was this article valuable?
Here are more articles you may enjoy.


 Fla. Commissioner Offers Major Changes to Citizens’ Commercial Clearinghouse Plan
Fla. Commissioner Offers Major Changes to Citizens’ Commercial Clearinghouse Plan  Insurance Broker Stocks Sink as AI App Sparks Disruption Fears
Insurance Broker Stocks Sink as AI App Sparks Disruption Fears  CFC Owners Said to Tap Banks for Sale, IPO of £5 Billion Insurer
CFC Owners Said to Tap Banks for Sale, IPO of £5 Billion Insurer  State Farm Adjuster’s Opinion Does Not Override Policy Exclusion in MS Sewage Backup
State Farm Adjuster’s Opinion Does Not Override Policy Exclusion in MS Sewage Backup 

