Over the past decade, the insurance industry has undergone an increasingly rapid transformation, driven by advancements in machine learning, artificial intelligence, and now generative AI technologies.
These advancements have enabled insurers to automate routine tasks such as data entry, document creation, and various aspects of underwriting and claims processes. Generative AI unlocks new potential by automating more complex tasks, allowing employees to focus on intricate aspects of risk assessment and claims management. This same technology allows insurers to rapidly discover insights from previously difficult-to-use sources of data, such as scanned documents and notes taken by claims adjusters. These insights can be used to identify previously unknown areas of concern and inform risk assessment and management efforts.
An often overlooked and valuable source of insurance data comes from unstructured data sources, but it has historically been an untapped resource. Unstructured data, such as claim notes, accident descriptions, scanned documents, images, audio, and video, often contains the most essential information about a worker’s injury, legal proceedings, and medical treatment.
This data has traditionally been challenging to analyze, often requiring bespoke AI models tailor-made by expensive data scientists and insurtech vendors. Generative AI, including large language models (LLMs) from OpenAI, Google, and Anthropic, represents a significant leap forward in the capability to understand and generate human-like text. Generative AI models can process unstructured data quickly and cost-effectively, often leading to key insights much faster than traditional methods.
The opportunities for harnessing AI in workers’ comp are immense. By effectively processing unstructured data, insurers can uncover patterns and trends that were previously hidden, reducing the time to insight and enhancing worker safety protocols. This capability not only improves the efficiency of claims analysis but also empowers insurers to anticipate and mitigate future risks, ultimately leading to safer workplaces and reduced claim costs.
Even though generative AI models are powerful and improving rapidly, they are not perfect, and they should not be used without acknowledging risks. Unstructured insurance data, especially in workers’ comp, often contains personally identifiable information and personal health information, as well as other sensitive subject matter. When working with this data, care must be taken to ensure all regulatory, data privacy, and information security policies are followed. Additionally, generative AI models are known to produce unpredictable inaccuracies known as “hallucinations.” While there are many techniques to reduce hallucinations from generative AI models, it is ultimately the responsibility of those using the technology to ensure the results of any AI-assisted analysis are accurate.
From Data Gaps to Clarity
To further illustrate the opportunities generative AI creates in transforming workers’ comp, we ran a series of experiments that showcase its practical application. This study leveraged secured generative AI and large LLMs to analyze unstructured data sources, such as claim notes and accident descriptions, to compare with the structured data (such as NCCI injury codes, diagnosis codes, and procedure codes). We had the goal of identifying root causes of injuries and safety concerns. The findings from the study offer a compelling look at how AI-driven analysis can empower insurers and employers to foster safer work environments and reduce claim costs.
The first experiment aimed to identify the true root causes of an injury. In a study of nearly 4 million claims across 70 workers’ comp claim source systems, we found that 15% of all causes of injury are missing or coded as miscellaneous. This does not include the significant number that are coded either incorrectly or less specifically than they should be. For example, an injury may be coded as a generic slip and fall instead of specifying that the slip was on ice or the fall was from a ladder.
Missing, inaccurate, and generic coding makes it difficult for insurance carriers and risk managers to identify the best ways to improve safety programs and practices. The same issues can be seen in the unstructured data captured at the first notice of loss. The aforementioned study also identified that 7% of the descriptions of the injury captured by claims adjusters do not contain an adequate description of the event. Instead, they contain descriptions like “No description on file,” “Not Provided,” “Unknown,” or a generic “Worker injured on site,” “Employee cut finger,” and “Needlestick.” The critical information about the specific circumstances that led to the injury is not present in the most easily analyzed text. It instead is often contained in notes taken by claims adjusters and stored in claims systems or documents scanned into imaging systems.
Prompting Precision in Claims
It will come as no surprise to anyone who has worked with multiple claims systems that the format in which this vital information is captured can vary widely. While some claims systems may utilize standardized templates for such details, for others the format may be at the discretion of individual adjusters.
Generative AI models excel at processing short passages of text and following simple instructions. In our experiment, we leveraged a secured LLM to “read” the claim notes for injuries related to several industries, including retail, academic, and public entities. By creating targeted prompts to identify root causes of injury and drill down on specific areas of interest, we were able to greatly reduce the number of claims with missing or inadequate injury coding. For a large university, we reduced the number of poorly coded injuries by 75% and identified the small handful of injuries where it is unclear what caused the injury. Additionally, we identified corrections or further clarifications to the injury coding for 30% of the injuries. For example, our generative AI process correctly determined that the injury of an injured worker who was burned when a hot cup of coffee was thrown at him should be coded as a burn instead of being struck by an object.
Improving the accuracy of the coded injury information across a population of claims enabled us to uncover additional insights that were not evident in the unenhanced data. For a retail account, we identified specific equipment that employees were repeatedly tripping over and shared this information with their risk management team. Additionally, we identified seasonality in a specific category of injuries that was previously unknown.
Before the release of robust LLMs such as ChatGPT in 2022, manually correcting injury coding by cross-referencing claim notes for 1,000 claims would have taken several days spread across weeks and required the expertise of experienced claims adjusters. By leveraging generative AI, we completed this task in a matter of hours for less than $100, engaging subject matter experts when needed. We have consistently found robust results by applying this technique to other claim attributes across various industries.
Illuminating Injury Context
In a subsequent experiment, we delved further into the nature of injuries to determine if they were avoidable or could have been made less severe with improved safety measures. This information is critical for developing robust risk management programs, yet it is typically not captured in a manner that is easily reportable.
As in the previous experiment, we leveraged a secured generative AI model to examine the claim notes taken by claims adjusters to identify key attributes related to the injury. In this study, we sought any indication that an injury was avoidable and analyzed the details of such injuries. For example, when analyzing injuries for a retail store, we easily distinguished cuts occurring from routine work, such as opening boxes or preparing food in the deli, from instances where injuries occurred due to improper procedures, like cleaning equipment while it is still running or not wearing proper safety gear. As in the first experiment, utilizing generative AI allowed us to extract these insights in a fraction of the time required for manual review. Not only do we use these insights to discuss the safety programs in place with employers in a data-driven manner, but we can also conduct this same analysis across peer employers to produce actionable benchmarking.
In addition to understanding the nuances of the injury, it is crucial to accurately capture detailed information about the department and job function of the injured worker. This allows employers to determine if there are systemic issues that can be addressed through targeted training or process improvement. In the aforementioned study of nearly 4 million claims, we found that more than 30% of claims did not have valid job class coding, and 25% of claims lacked a free-text occupational description.
Even for claims where structured data is available, the information is often vague. For example, an employee’s occupation may be listed as “SCHOOLS-ALL OTHER” or “MUNICIPAL EMPLOYEE,” which does not indicate the specifics of the employee’s job function or where the risk of injury may reside in their role. By leveraging generative AI in the manner described, we were able to derive the occupation of the injured employee and further classify their occupation. For example, in a large university, we quickly processed thousands of jobs labeled “SCHOOLS-ALL OTHER.” We identified which employees were teachers, janitorial staff, cafeteria workers, grounds crew, medical staff at the university hospital, or administrative staff. We are now able to analyze trends and derive insights specific to the particular job functions and compare them across multiple employers.
Human Oversight Remains Essential
The utilization of generative AI in claims processing is not just a technological advancement; it represents a fundamental shift in how insurers can approach risk management. By automating and refining the analysis of unstructured data, insurers can uncover insights that were previously obscured by vague or incomplete information. This information can be used for claims handling, underwriting, and risk management.
While the benefits of generative AI are evident, it is crucial to reiterate that these models are not perfect and can produce inaccurate results. In our experiments, all insights were manually reviewed for accuracy. Although we generally found generative AI models to be highly accurate for our use cases, they were not without error. Insurers must exercise caution and ensure that AI-generated insights are carefully reviewed and validated. Relying solely on AI without human oversight may result in misguided conclusions and poor decisions.
A balanced approach that combines AI efficiency with expert judgment is essential for optimizing claims handling and risk management strategies.
As generative AI continues to evolve, its role in transforming the insurance industry will undoubtedly expand. Claims professionals who embrace this technology and integrate it thoughtfully into their operations will be better positioned to anticipate risks and improve their internal operations.
This article first appeared on ClaimsJournal.com, a sister publication to Insurance Journal.
Topics InsurTech Data Driven Artificial Intelligence Workers' Compensation Talent
Was this article valuable?
Here are more articles you may enjoy.



 Marine Insurers Cancel War Risk Cover as Iran Conflict Escalates
Marine Insurers Cancel War Risk Cover as Iran Conflict Escalates  Florida Appeals Court Pulls the Plug on Physician Dispensing in Workers’ Comp
Florida Appeals Court Pulls the Plug on Physician Dispensing in Workers’ Comp 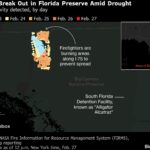 Deep Freeze and Drought Fueled a Massive Florida Wildfire
Deep Freeze and Drought Fueled a Massive Florida Wildfire  Zurich Insurance Said to Near Beazley Deal Funded by Equity Sale
Zurich Insurance Said to Near Beazley Deal Funded by Equity Sale